“By using a polyvagal perspective, we can give up self-criticism and open our hearts to exploring our everyday experiences” – Deb Dana, LCSW
Dr. Stephen Porges, originator of Polyvagal Theory, identified a biological order of human response that is active in all human experience. With gratitude to Dr. Porges for his work, this handout explores and explains Polyvagal Theory in user-friendly language.
We come into the world wired to connect. With our first breath, we embark on a quest to feel safe in our bodies, in our environments, and in our relationships with others. The autonomic nervous system is our personal surveillance system, always on guard, asking the question “Is this safe?” Its goal is to protect us by sensing safety and risk, listening moment by moment to what is happening in and around our bodies and in the connections we have to others.
This listening happens far below awareness and far away from our conscious control. Dr. Porges, understanding that this is not awareness that comes with perception, coined the term neuroception to describe the way our autonomic nervous system scans for cues of safety, danger, and life threat without involving the thinking parts of our brain. Because we humans are meaning-making beings, what begins as the wordless experiencing of neuroception drives the creation of a story that shapes our daily living.
The Autonomic Nervous System – Anatomy and Abilities
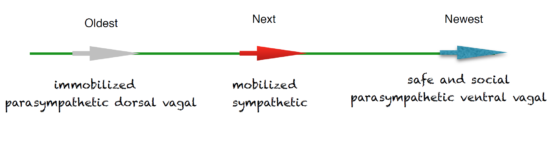
The autonomic nervous system is made up of two main branches, the sympathetic and the parasympathetic, and responds to signals and sensations via three pathways, each with a characteristic pattern of response. Through each of these pathways, we react “in service of survival.”
The sympathetic branch is found in the middle part of the spinal cord and represents the pathway that prepares us for action. It responds to cues of danger and triggers the release of adrenaline, which fuels the fight-or-flight response.
In the parasympathetic branch, the remaining two pathways are found in a nerve called the vagus. Vagus, meaning “wanderer,” is aptly named. From the brain stem at the base of the skull, the vagus travels in two directions: downward through the lungs, heart, diaphragm, and stomach and upward to connect with nerves in the neck, throat, eyes, and ears.
The vagus is divided into two parts: the ventral vagal pathway and the dorsal vagal pathway. The ventral vagal pathway responds to cues of safety and supports feelings of being safely engaged and socially connected. In contrast, the dorsal vagal pathway responds to cues of extreme danger. It takes us out of connection, out of awareness, and into a protective state of collapse. When we feel frozen, numb, or “not here,” the dorsal vagus has taken control.
Dr. Porges identified a hierarchy of response built into our autonomic nervous system and anchored in the evolutionary development of our species. The origin of the dorsal vagal pathway of the parasympathetic branch and its immobilization response lies with our ancient vertebrate ancestors and is the oldest pathway. The sympathetic branch and its pattern of mobilization, was next to develop. The most recent addition, the ventral vagal pathway of the parasympathetic branch brings patterns of social engagement that are unique to mammals.
When we are firmly grounded in our ventral vagal pathway, we feel safe and connected, calm and social. A sense (neuroception) of danger can trigger us out of this state and backwards on the evolutionary timeline into the sympathetic branch. Here we are mobilized to respond and take action. Taking action can help us return to the safe and social state. It is when we feel as though we are trapped and can’t escape the danger that the dorsal vagal path- way pulls us all the way back to our evolutionary beginnings. In this state we are immobilized. We shut down to survive. From here, it is a long way
back to feeling safe and social and a painful path to follow.
The Autonomic Ladder
Let’s translate our basic knowledge of the autonomic nervous system into everyday understanding by imagining the autonomic nervous system as a ladder. How do our experiences change as we move up and down the ladder?

Ventral Vagal
Sympathetic
Dorsal Vagal
The Top of the Ladder
What would it feel like to be safe and warm? Arms strong but gentle. Snuggled close, joined by tears and laughter. Free to share, to stay, to leave… 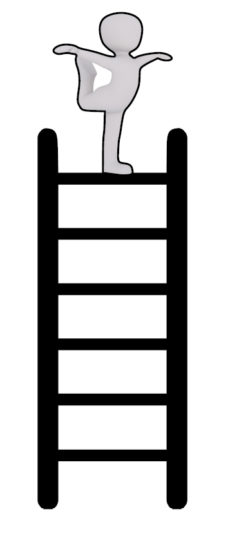
Safety and connection are guided by the evolutionarily newest part of the autonomic nervous system. Our social engagement system is active in the ventral vagal pathway of the parasympathetic branch. In this state, our heart rate is regulated, our breath is full, we take in the faces of friends, and we can tune in to conversations and tune out distracting noises. We see the “big picture” and connect to the world and the people in it. I might describe myself as happy, active, interested and the world as safe, fun, and peaceful. From this ventral vagal place at the top of the autonomic ladder, I am connected to my experiences and can reach out to others. Some of the daily living experiences of this state include being organized, following through with plans, taking care of myself, taking time to play, doing things with others, feeling productive at work, and having a general feeling of regulation and a sense of management. Health benefits include a healthy heart, regulated blood pressure, a healthy immune system decreasing my vulnerability to illness, good digestion, quality sleep, and an overall sense of well-being.
Moving Down the Ladder
Fear is whispering to me and I feel the power of its message. Move, take action, escape. No one can be trusted. No place is safe…
 The sympathetic branch of the autonomic nervous system activates when we feel a stirring of unease—when something triggers a neuroception of danger. We go into action. Fight or flight happens here. In this state, our heart rate speeds up, our breath is short and shallow, we scan our environment looking for danger—we are “on the move.”
The sympathetic branch of the autonomic nervous system activates when we feel a stirring of unease—when something triggers a neuroception of danger. We go into action. Fight or flight happens here. In this state, our heart rate speeds up, our breath is short and shallow, we scan our environment looking for danger—we are “on the move.”
I might describe myself as anxious or angry and feel the rush of adrenaline that makes it hard for me to be still. I am listening for sounds of danger and don’t hear the sounds of friendly voices. The world may feel dangerous, chaotic, and unfriendly. From this place of sympathetic mobilization—a step down the autonomic ladder and backward on the evolutionary timeline I may believe, “The world is a dangerous place and I need to protect myself from harm.” Some of the daily living problems can be anxiety, panic attacks, anger, inability to focus or follow through, and distress in relationships. Health consequences can include heart disease; high blood pressure; high cholesterol; sleep problems; weight gain; memory impairment; headache; chronic neck, shoulder, and back tension; stomach problems; and increased vulnerability to illness.
The Bottom of the Ladder
I’m far away in a dark and forbidding place. I make no sound. I am small and silent and barely breathing. Alone where no one will ever find me… 
Our oldest pathway of response, the dorsal vagal pathway of the parasympathetic branch, is the path of last resort. When all else fails, when we are trapped and action taking doesn’t work, the “primitive vagus” takes us into shutdown, collapse, and dissociation.
Here at the very bottom of the autonomic ladder, I am alone with my despair and escape into not knowing, not feeling, almost a sense of not being. I might describe myself as hopeless, abandoned, foggy, too tired to think or act and the world as empty, dead, and dark. From this earliest place on the evolutionary timeline, where my mind and body have moved into conservation mode, I may believe, “I am lost and no one will ever find me.”
Some of the daily living problems can be dissociation, problems with memory, depression, isolation, and no energy to do the tasks of daily living. Health consequences of this state can include chronic fatigue, fibromyalgia, stomach problems, low blood pressure, type 2 diabetes, and weight gain.
Daily Movements on the Ladder
Now that we’ve explored each of the places on the autonomic ladder, let’s consider how we move up and down. Our preferred place is at the top of the ladder. As the song “I Can See Clearly Now” (written by Johnny Nash) says, “I can see clearly now, the rain is gone. I can see all obstacles in my way. Gone are the dark clouds that had me blind.”
The ventral vagal state is hopeful and resourceful. We can live, love, and laugh by ourselves and with others. This is not a place where everything is wonderful or a place without problems. But it is a place where we have the ability to acknowledge distress and explore options, to reach out for support and develop organized responses. We move down the ladder into action when we are triggered into a sense of unease—of impending danger. We hope that our action taking here will give us enough space to take a breath and climb back up the ladder to the place of safety and connection. It is when we fall all the way down to the bottom rungs that the safety and hope at the top of the ladder feels unreachable.
What might a real-life example of moving up and down the autonomic ladder look like?
Consider the following two scenarios.
I am driving to work in the morning listening to the radio and enjoying the beginning of the day (top of the ladder) when a siren sounds behind me (quick move down the ladder). I feel my heart race and immediately worry that I’ve done something wrong (staying in my spot down the ladder). I pull over and the police car rushes by me. I pull back out and resume my drive to work and feel my heart begin to return to its normal speed (moving up the ladder). By the time I get to work, I have forgotten about the incident and am ready for my day (back at the top of the ladder).
I am having dinner with friends enjoying the conversation and the fun of being out with people I like (top of the ladder). The conversation turns to vacations, and I start comparing my situation to my friends’ situations. I begin to feel angry that I can’t afford a vacation, that my job doesn’t pay enough, that I have so many unpaid bills I’ll never be able to take a vacation (moving down the ladder). I sit back and watch as my friends continue to talk about trips and travel planning. I disconnect from the conversation and begin to feel invisible as the talk goes on around me (shutting down and moving to the bottom of the ladder). The evening ends with my friends not noticing my silence and with me feeling like a misfit in the group (stuck at the bottom of the ladder). I go home and crawl into bed (the only place I know now is the bottom of the ladder).
The next morning, I wake up and don’t want to get up or go to work (still at the bottom of the ladder). I worry I’ll get fired if I don’t show up and drag myself out of bed (a bit of energy and beginning of movement up the ladder). I am late to work. My boss comments on my lateness, and I have a hard time holding in an angry response (continuing to move up the ladder with more mobilized energy). I decide I’ve had enough of this job and will seriously look for a new one (still moving up the ladder). I begin to consider the skills I can bring to a new job and that with the right job I will be able to pay my bills and maybe even take a vacation. I have lunch with a coworker, and we talk about our jobs and dreams for the future (back at the top of the ladder).
Systems Working Together
We experience well-being when the three parts of our autonomic nervous system work together. To understand this integration, we leave the imagery of the ladder and imagine instead a home.
The dorsal vagal system runs the “basic utilities” of the home. This system works continually in the background keeping our basic body systems online and in order. When there is a glitch in the system, we pay attention. When all is running smoothly, the body’s functions work automatically. Without the influence of the ventral vagal system, the basic utilities run the empty house, but “no one is home.” Or, if we are home, the environment is one that brings no comfort. Everything is turned down to the lowest possible setting—enough to keep the air circulating and the pipes from freezing. The environment is just habitable enough to sustain life.
The sympathetic branch can be thought of as the home security system maintaining a range of responses and armed to react to any emergencies. This alarm system is designed to trigger an immediate response and then return to standby. Without the influence of the ventral vagal system, the alarm system receives a steady stream of emergency notifications and continues to sound the alarm.
The ventral vagal system allows us to soak in, and savor, this home we are inhabiting. We can enjoy it as a place to rest and renew by ourselves and as a place to join with friends and family. We feel the “basic utilities” running in the background. The rhythms of our heart and breath are regulated. We trust that the “monitoring system” is on standby. The integration of systems allows us to be compassionate toward others, curious about the world we live in, and emotionally and physically connected to others.
Where Do We Go Next?
With this initial understanding of the role and responses of the autonomic nervous system in service of our safety and survival, we can begin to befriend the autonomic nervous system and map our personal response patterns. The befriending skills lead to attending practices. Our mapping leads naturally to tracking. With the awareness of tracking, we can begin to intentionally tune and tone our autonomic nervous system. We can successfully navigate our quest for safety and connection.
I invite you to my practice and to benefit from the craniosacral therapy sessions if you feel that your autonomic nervous system needs support. If you have any questions, please do not hesitate to contact me: kontakt@exploreself.pl
Agnieszka
Copyright Deb Dana 2018, A BEGINNER’S GUIDE TO POLYVAGAL THEORY.
Source: The Rythm of Regulation